The US is experiencing its worst year for measles in over three decades, with more than 1,300 cases in 40 states as of July 16. Cases were almost as high in 2019, putting the country’s measles elimination status at risk. Six years ago, health officials were able to stop the spread. But amid growing public backlash against vaccines, many of the tactics used then may not work now.
Measles elimination means there has been no continuous transmission in a country for longer than 12 months. That almost happened in the 2019 outbreak, which largely affected Orthodox Jewish populations in New York City and some surrounding counties. In fall 2018, US travelers returning from Israel tested positive for measles. The disease quickly spread throughout close-knit communities, especially among children, due to low vaccination rates. While the statewide measles vaccination rate for school-age children was 98 percent the previous school year, vaccination coverage in schools in the outbreak area was only 77 percent. Because measles is highly contagious, a 95 percent vaccination rate is needed to protect a community from the disease.
As a result, the majority of measles cases occurred in individuals 18 and under, nearly 86 percent of whom were known to be unvaccinated. Some of those people developed severe complications, including pneumonia, and nearly 8 percent were hospitalized.
The current surge is being fueled by an outbreak that started in an undervaccinated Mennonite community in West Texas. Cases have since spread to other Texas counties, New Mexico, and Oklahoma. Two children in Texas with no underlying conditions and one adult in New Mexico have died this year as a result of measles. All were unvaccinated.
“There are definitely parallels. What we saw in New York was very much the result of years and years of spread of misinformation and disinformation around the safety of vaccines,” says Neil Vora, executive director of Preventing Pandemics at the Source Coalition and previously a medical epidemiologist at the Centers for Disease Control and Prevention who helped respond to the 2019 outbreak.
Cases eventually burned out in New York after a months-long effort that included both traditional public health approaches and policy changes at the local and state level.
“You need to take the first case seriously, because it’s like kindling. You never know when that fire is just going to break out,” says Oxiris Barbot, the current president and CEO of the United Hospital Fund, who served as New York City’s health commissioner from 2018 to 2020.
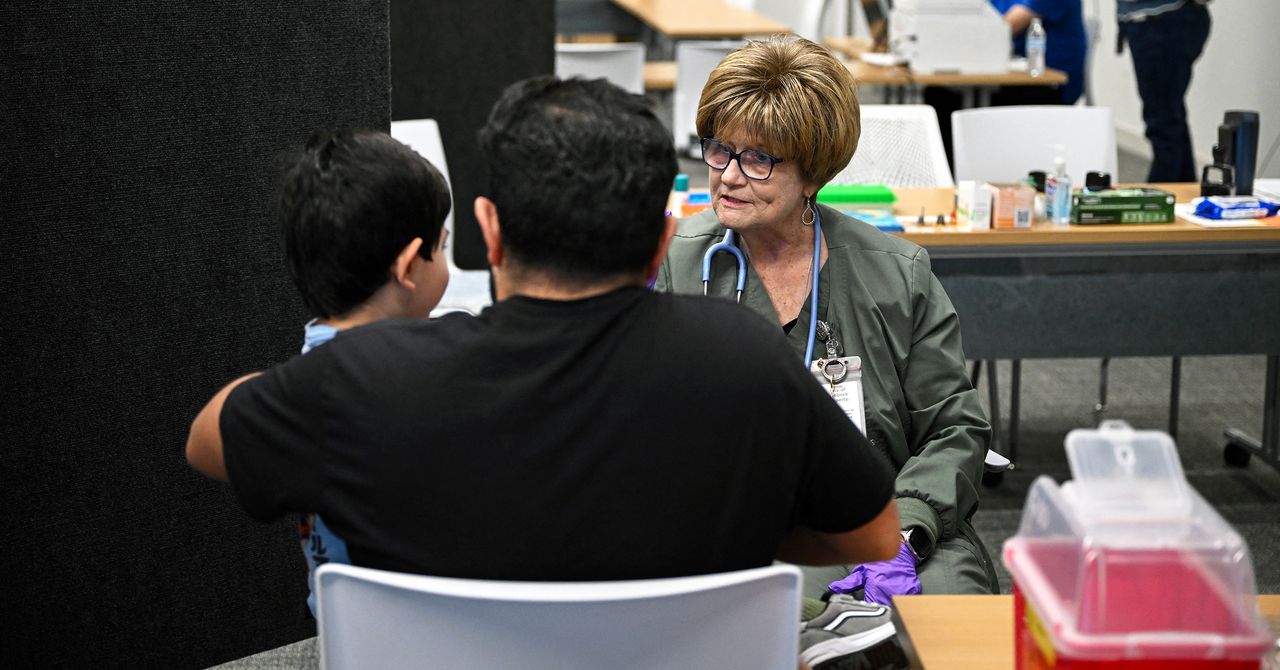
As the disease spread, Barbot realized the city health department would need to go to the source of transmission, largely the Orthodox Jewish schools in affected neighborhoods. Working with school administrators, they reviewed vaccination records to identify unvaccinated or under-vaccinated children. Following an exposure, those children were prohibited from attending school and childcare for 21 days, the incubation period for measles. Similar measures were taken in some counties outside the city.
“It took a lot of staff time, a lot of leg work,” Barbot says. In one school, a contagious child led to more than 25 infections in other students and further spread outside the school. She says the health department was “heavily involved” in making sure schools were abiding by the quarantine measures.”