Health Secretary Robert F. Kennedy Jr. is pushing for doctors to receive more education about nutrition.
He announced Wednesday that a team within the Health and Human Services Department would target “the woeful lack of nutrition education in medicine” by making it a greater part of premed and medical school curricula, medical licensing exams, residencies, board certification and doctors’ continuing education.
“We can reverse the chronic disease epidemic simply by changing our diets and lifestyles, but to do that, we need nutrition to be a basic part of every doctor’s training,” Kennedy said in a video on X. “We’ll start by embedding nutrition directly into college premed programs and test it on the MCAT.”
The move comes as Kennedy has taken far more controversial steps to reshape public health in America, including slashing vaccine research and downsizing federal health agencies.
HHS did not respond to individual questions, but pointed NBC News to a press release.
The department has directed medical education organizations to submit written plans for incorporating nutrition education by Sept. 10. The Association of American Medical Colleges creates the Medical College Admission Test (MCAT), and medical schools have requirements or recommendations for the coursework that premed students should take.
Many doctors lauded the announcement for recognizing the role of nutrition in managing and preventing chronic disease, a personal interest of Kennedy’s that he has made a policy priority in office. However, some expressed concern about not having enough time in the exam room to provide nutrition counseling, and said HHS’ resources would be better spent incentivizing hospitals to have more dietitians on staff or expanding insurance coverage for dietary counseling. Still others said Kennedy’s announcement undermines trust in doctors and sows doubt in their ability to care for patients.
Texas and Louisiana both passed laws in June that align with Kennedy’s medical education policy proposals. Texas’ law requires doctors to take nutrition courses to renew their licenses and medical schools to offer nutrition education to receive certain public funds. Louisiana’s law requires some doctors to complete a minimum of one hour of continuing education in nutrition every four years.
Dr. Nate Wood, a primary care physician and the director of culinary medicine at Yale School of Medicine, said the idea that doctors should be well-trained in nutrition is a good one. However, he doubted whether it was the most effective approach to fighting chronic disease.
“I think it’s a little short-sighted to think that physicians are going to be the answer to this chronic disease epidemic by providing nutrition counseling,” he said.
Wood added that “a lot of visits are sick visits, where patients come in for a very quick visit and they want to address four or more complex problems, and it’s already very difficult to address even one or two of those.”
In an editorial in The Wall Street Journal on Wednesday, Kennedy said medical organizations “look the other way” when it comes to nutrition education requirements. He pointed to a 2022 survey in the Journal of Wellness, which suggests that medical students receive just over an hour of formal nutrition education per year, on average. He also cited a 2024 study in the journal Advances in Nutrition, which found that 75% of U.S. medical schools have no required clinical nutrition classes.
Previously, Kennedy said he would withhold funding for medical schools that didn’t have nutrition courses.
“That’s what really inspired me to get into this field, seeing that nutrition was the top cause of poor health in most of my patients, yet it was pretty much missing from my education,” Dr. Dariush Mozaffarian, a cardiologist who directs the Food is Medicine Institute at Tufts University.
He said he supports Kennedy’s policy proposals for nutrition education in medicine.
“The federal government should say, ‘Look, if you’re not going to do your job and train doctors how they should be trained, we’re going to stop funding you.’ And then they’ll listen,” Mozaffarian said.
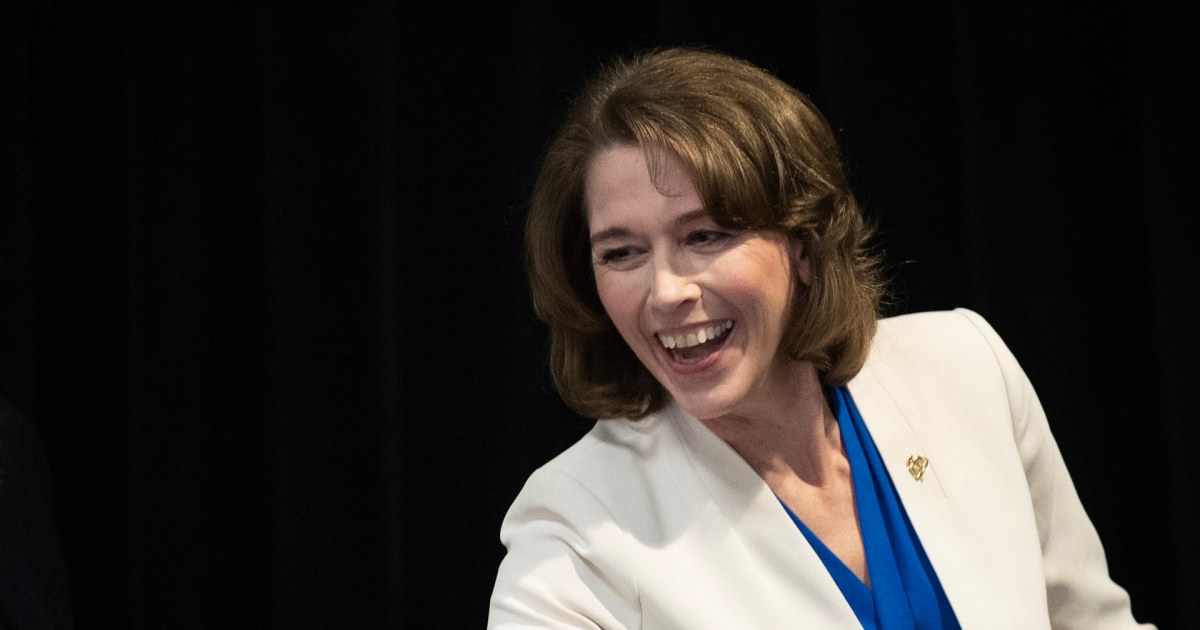
But the Association of American Medical Colleges maintains that medical students are trained about the impact of diet on health. According to the group’s recent survey of U.S. and Canadian medical schools, all 182 schools said they cover nutrition as part of their required curricula, up from 89% five years earlier.
“Medical schools understand the critical role that nutrition plays in preventing, managing, and treating chronic health conditions, and incorporate significant nutrition education across their required curricula,” Alison Whelan, the chief academic officer of the AAMC, said in a statement.
Kennedy’s call for more nutrition education has sparked debate about what people can reasonably expect of primary care doctors.
Mozaffarian said the goal is not to turn doctors into dietitians, but to give them enough knowledge to identify issues with a patient’s diet and refer that person to a specialist.
However, Dr. Jake Scott, an infectious diseases specialist at Stanford Medicine, said doctors have that basic knowledge already.
“We’re not ignorant when it comes to nutrition, and that’s the implication” of Kennedy’s announcement, he said.
Scott added that poor nutrition in the U.S. is not just a problem with not knowing that quinoa is healthier than fries. It’s also a product of systemic barriers, such as being unable to afford a doctor or access healthy foods, he said. Around 18.8 million people in the U.S. live in food deserts — low-income neighborhoods far away from a supermarket.
“There’s so many other creative, possible solutions, but tacking on this medical education requirement, it’s the last thing I would do if I were the head of HHS,” he said.
Wood said an alternative solution would be a greater push to get dietitian appointments covered by insurance. For example, while these visits can be covered under Medicare, they typically require a patient to either be diabetic or have kidney disease. Coverage for patients with private insurance and Medicaid can vary, he said.