The U.S. Food and Drug Administration (FDA) will no longer recommend yearly COVID-19 vaccines for kids and most adults.
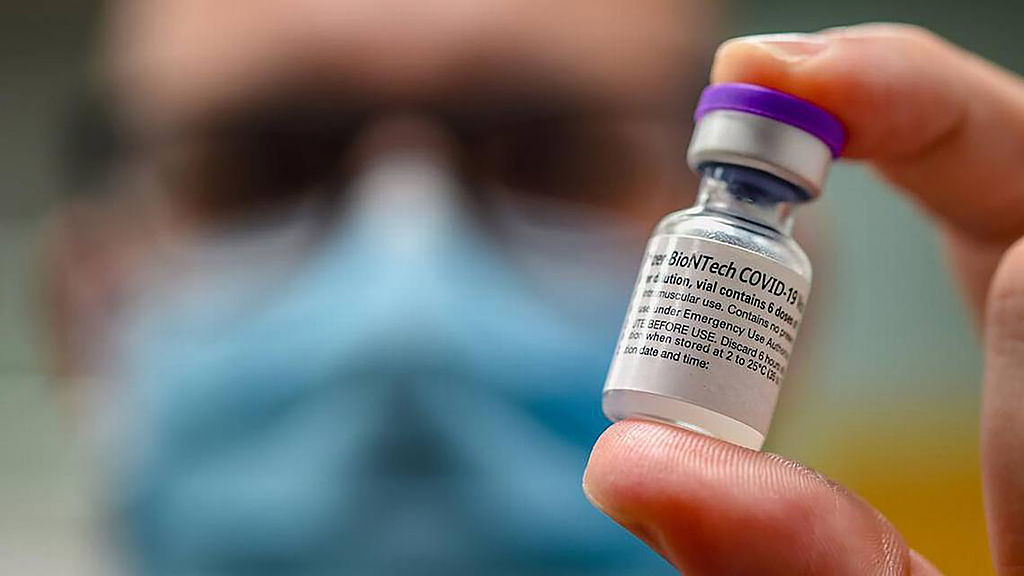
In an editorial article published in the New England Journal of Medicine, Dr. Vinay Prasad, the newly appointed head of the Center for Biologics Evaluation and research at the FDA, and Dr. Martin Makary, FDA commissioner, explained their plan for how the FDA will evaluate and recommend COVID-19 vaccines going forward.
Until now, federal guidance has recommended that everyone six months or older receive a COVID-19 vaccine targeting the latest circulating version of the virus to maximize their chances of avoiding severe disease.
The new FDA leadership still recommends that groups at higher risk of being hospitalized or dying from COVID-19 receive yearly COVID-19 shots. This includes seniors, adults with weakened immune systems, and people with underlying health conditions like cancer. Some people in these groups may even qualify for a second shot in a given year, depending on their risk factors.
But for people at lower risk, the FDA leadership is instead pushing for additional studies to test whether people in the general population who get an annual shot have fewer COVID-19 symptoms, less-severe cases, and fewer hospitalizations and deaths compared to those receiving a placebo. Pfizer-BioNTech, Moderna, and Novavax, which make the COVID-19 vaccines, did not immediately respond to a request for comment about the changes.
“We simply don’t know whether a healthy 52-year old woman with a normal BMI who has had COVID-19 three times and has received six previous doses of a COVID-19 vaccine will benefit from the seventh dose,” Prasad and Makary write in the editorial. “This policy will compel much-needed evidence generation.”
Read More: How Having a Baby Is Changing Under Trump
Prasad and Makary write that the proposed studies would not interfere with the current timeline of approving the yearly COVID-19 vaccines, since they would be conducted after the vaccine is released in what the agency calls post-marketing studies. The FDA’s advisory committee of experts is meeting on May 22 to review data from the World Health Organization about which variants to target in next season’s vaccine, which would be distributed in the fall.
Even if the additional studies won’t delay the availability of the next COVID-19 shot, they would place an additional burden on pharmaceutical companies to conduct another trial, which could add to the cost of the vaccine for the public, says Dr. Paul Offit, a member of that FDA advisory committee and professor at Children’s Hospital of Philadelphia.
Another challenge is that in order to conduct this type of trial, some people would have to receive a placebo and therefore potentially be less protected from COVID-19. “Anybody can catch this virus and be hospitalized and killed,” Offit says. “We know the vaccine works and probably saved three million lives, and we know that the virus is still circulating and still causes harm.” Because of that continued risk, he says it’s not clear whether an institutional review board—which evaluates all study designs involving human volunteers—would consider this an ethical trial.
Offit acknowledges that for most people who are not at high risk of severe disease, and who by now have had at least one, if not several, bouts of COVID-19, getting a yearly vaccine is “low risk, low reward.” Studies from the CDC show that the shot boosts antibodies that fight the virus for about four to six months, providing strong protection against mild-to-moderate disease during that time, but then that protection wanes. Different immune cells, T cells, continue to protect against severe disease, hospitalization, and death, which is another reason to stay up to date on the vaccine.
Even the shorter term protection, however, may be worth it to avoid illness. “You buy yourself four to six months of protection from mild-to-moderate disease, which is not trivial,” he says, especially as more data suggests that repeated bouts of COVID-19 could contribute to more intense and lasting symptoms of Long COVID.