Earlier this month, the Trump administration said it was terminating $500 million in mRNA vaccine research and shifting its focus to other approaches, including a previously announced “whole-virus” vaccine platform dubbed “Generation Gold Standard.”
“Generation Gold Standard is a paradigm shift,” Dr. Jay Bhattacharya, the director of the National Institutes of Health, said in a news release in May touting the next research initiative. “It extends vaccine protection beyond strain-specific limits and prepares for flu viral threats — not just today’s, but tomorrow’s as well — using traditional vaccine technology brought into the 21st century.”
Vaccine and infectious disease experts, however, say the approach is misguided.
“It’s somewhat of a step backward,” said Dr. James Campbell, vice chair of the American Academy of Pediatrics Committee on Infectious Diseases. “We’ve had inactivated whole-virus vaccines for a very, very long time.”
The first whole-virus vaccine was developed in the late 1800s by Louis Pasteur, who made an early version of the rabies vaccine.
“It’s not innovative at all,” said Angela Rasmussen, a virologist at the University of Saskatchewan. “It’s actually ancient, sort of, by vaccine standards.”
Whereas other vaccines activate the immune system using specific proteins in viruses, whole-virus vaccines typically preserve most components of the viruses.
“You take the virus, grow it up, purify it and kill it with an inactivating agent. That’s a whole-killed viral vaccine,” said Dr. Paul Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia. Other whole-virus vaccines use live but weakened versions of viruses.
Campbell said that over many years of vaccine research, scientists have been able to identify the parts of a virus that are likeliest to activate the immune system and train it to fight back against an invading pathogen. Those parts are known as “antigens.”
If the immune system is like the body’s bloodhound, tracking down invaders, then many newer vaccine technologies that target specific antigens present the bloodhound with just the pieces of the invader’s clothes that are most helpful to it. A whole-virus vaccine, on the other hand, would instead be like presenting a bloodhound with an invader’s entire wardrobe.
Campbell said that it may sound better at first glance to use the whole virus rather than key pieces of it but that additional pieces of the virus might not actually do anything to improve the immune response.
“For example, hepatitis B vaccine is one antigen, the hepatitis B surface antigen, and it is almost 100% protective against hepatitis B. You do not need the whole hepatitis B virus,” he said.
Offit agreed. “The hepatitis B vaccine has virtually eliminated hepatitis B infections in young children,” he said. “So that’s good enough.”
Campbell offered Covid-19 vaccines as another example. “There were whole-virus Covid vaccines, but they weren’t used in the United States, they were used elsewhere, and if you look at the general protection from them, it’s not as good,” he said.
A study from Singapore, for instance, found that people who got a whole-virus Covid vaccine were more than 1.5 times to twice as likely to be infected than those who had been immunized with an mRNA vaccine that targeted only the virus’ spike protein.
“If killed whole-virus vaccines for Covid were thought to be the best technology to move forward with back when the pandemic started, we would have,” Campbell said.
Improperly deploying whole-virus vaccines when they aren’t needed isn’t just unnecessary; in some cases, it can be harmful.
Campbell pointed to the development of the RSV vaccine as a case in point.
“When we used whole-virus killed RSV vaccine many years ago, rather than protect children from RSV, it led to what we call ‘antibody-dependent enhancement,’” he said. “Children had a worse RSV than if they had not been vaccinated, and that was because they had formalin-inactivated whole-virus.”
That RSV vaccine trial was in the 1960s, and it set research back decades.
Ever since then, Campbell said, RSV vaccination has either been directed only against the F protein, a piece of the virus, or it has used a monoclonal antibody, which is like a preformed immune response. The first RSV vaccine was approved in 2023.
“Those protect really well,” he said. “We do not want to use whole-virus killed vaccine for RSV. It will hurt people.”
Some whole-virus vaccines are still used. The hepatitis A and rabies vaccines are killed whole-virus vaccines, meaning they include the constituent pieces of the virus that have been inactivated. Seasonal flu vaccines also use whole-virus technology.
Campbell said it’s possible that a whole-virus vaccine could be an optimal choice for some pathogens in the future.
In pursuit of a universal flu vaccine
But as for whether the whole-virus platform will unlock new innovation in the pursuit of a universal flu vaccine, as suggested by the Department of Health and Human Services, Campbell said that it would be possible to use whole-virus vaccines if they could be genetically engineered to express multiple flu strain antigens but that it doesn’t have much to do with the whole-virus platform.
“If it’s just whole-virus, and it’s one strain, that’s what we do now,” Campbell said.
Emily Hilliard, the press secretary for HHS, said in a statement: “Generation Gold Standard marks a critical step in restoring strategic focus and radical transparency to America’s pandemic preparedness.”
“Developed entirely by government scientists — free from industry influence — the BPL vaccine platform could provide broad, long-lasting protection against all influenza viral pathogens, including influenza and coronaviruses, with the added potential to block transmission and stop outbreaks at the source,” Hilliard said. BPL, or beta-propiolactone, is a chemical that has been used for decades to kill the viruses used in vaccines.
A universal flu vaccine has been a longtime goal of scientists, as it would ideally offer yearslong protection against the flu. Because of how quickly the virus mutates, yearly flu shots are needed to protect against the most current strains.
“There’s a lot of different avenues that people are working, and if we choose only one of those — especially one that’s a very old technology that people have tried so many times before and failed to make a universal flu vaccine — I think it’s putting all our eggs in one basket and not really moving the field along,” Campbell said.
Offit said withdrawing research funding for mRNA vaccines could be particularly harmful in the event of a pandemic.
“If something bad happens, like there is a bird flu pandemic, for example, we will be less prepared,” he said, adding that mRNA technology has a shorter production cycle than whole-killed virus vaccines, meaning an mRNA vaccine would be available much sooner.
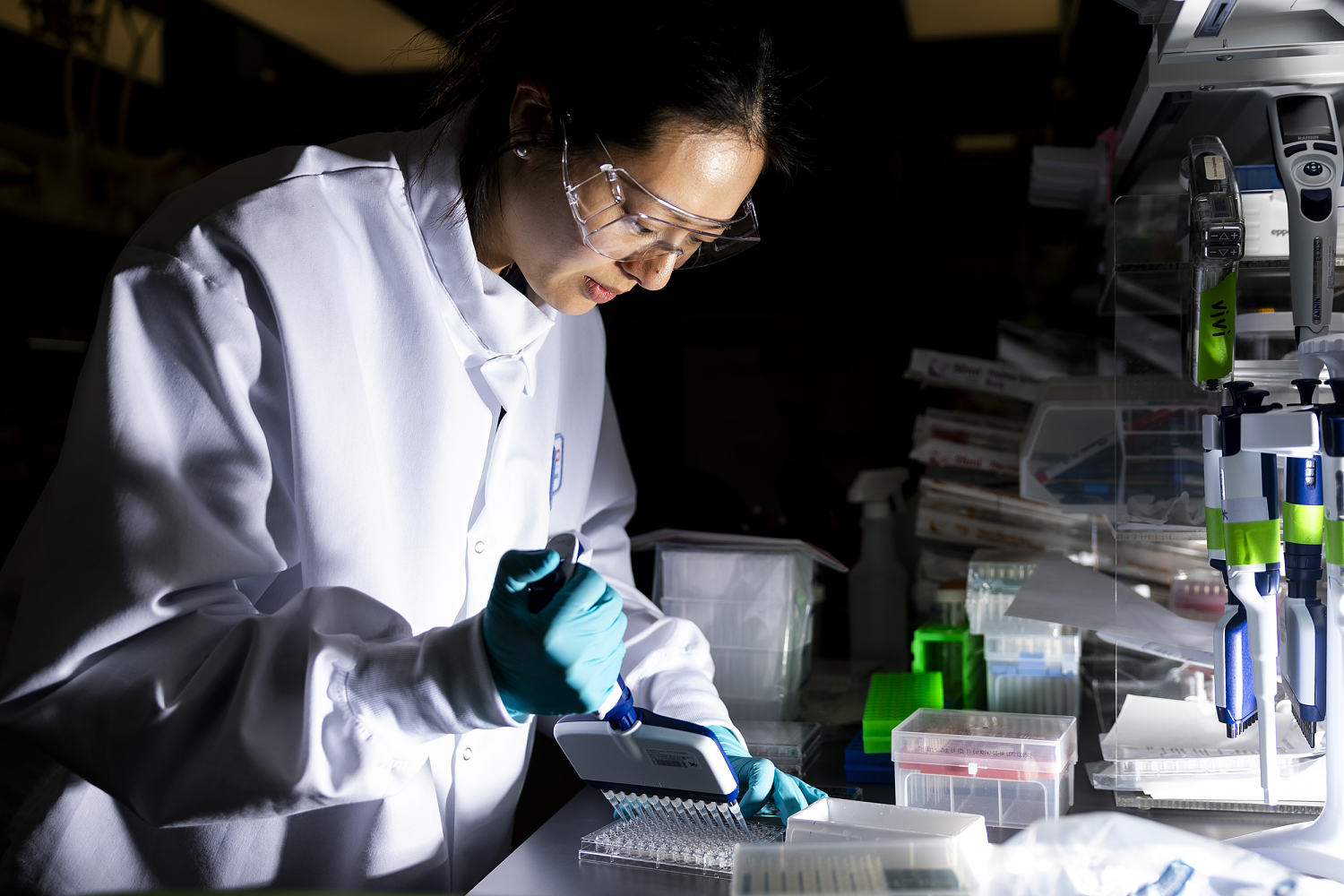
Rasmussen said, “We’d probably need a year to scale to full national scale manufacturing” using a whole-virus vaccine, adding, “You actually have to grow a ton of virus and then inactivate it and then make sure it’s inactivated.”
With other vaccine technologies, like protein subunit or mRNA, “you basically just make the protein or the mRNA, which can be done synthetically, without requiring any virus or anything to grow it in,” she said. “They’re much easier to change and adapt as needed, as new strains might emerge.”
Offit said, “One of the studies among the 22 studies that were eliminated in that $500 million withdrawal was looking at to what extent the mRNA technology would be valuable for bird flu.”
Ultimately, Campbell said, science should lead the way, not top-down dicta that tie scientists’ hands.
“The devil is in the details, not just in sweeping statements about what platform is an appropriate platform and which is not,” he said.
Multiple platforms are available for vaccine development, which are tested for their respective properties.
“Eventually, one or two, maybe, rise to look the best, and those are the ones that people continue to pursue,” he said. “That’s what we do in vaccinology, is try to figure out what works and what doesn’t work, both by basic science, by immunology, by models of diseases, before they get into humans, and then actual human studies to compare and contrast immune responses, safety and protection, not just sweeping statements about platform.”