Your gut-brain axis, hunger hormones, and environment work together to determine when you eat and when you stop.
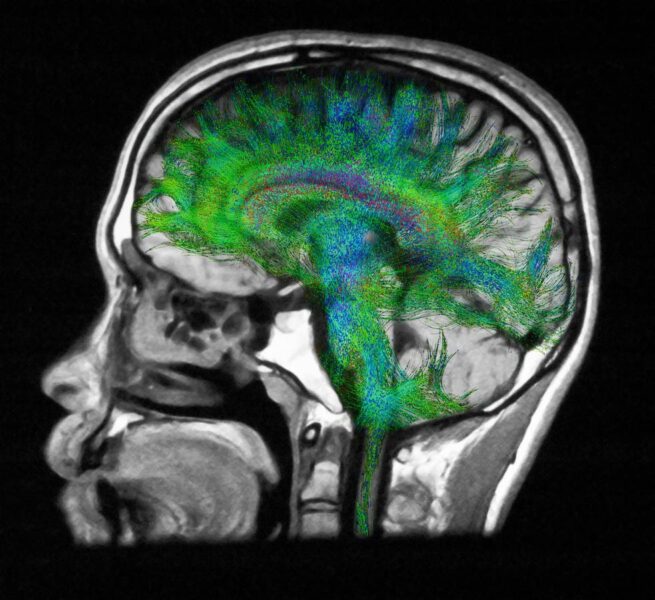
Diffusion MRI of the brain.
getty
Questions about hunger and fullness come up constantly in my clinic. Many patients try to manage appetite through willpower alone, without realizing how many powerful biological systems are influencing their hunger and fullness.
Every time you eat, or choose not to, you are responding to a sophisticated communication network between your gut, brain, hormones, and environment. This system determines when you feel hungry, how intensely you crave food, and when you feel full. Understanding how these short-term appetite signals work is the first step to understanding how your body regulates hunger, fullness, and weight.
This article is the first in a five-part Forbes Health series examining the biological systems that control hunger and fullness, how they influence long-term weight regulation, why they sometimes go awry, and how they can be targeted with modern treatments.
Key Concepts in Appetite Control
Before diving into the physiology, it is helpful to clarify a few core concepts. Appetite control involves two related but distinct processes. Satiation is the set of signals that tell you to stop eating during a meal. Satiety refers to the feeling of fullness and reduced appetite that persists after a meal and delays the return of hunger.
Another important distinction is between homeostatic hunger, which reflects true energy needs, and hedonic hunger, which is driven by the brain’s reward systems and can lead to eating for pleasure rather than necessity.
These concepts frame how the gut, brain, and hormones interact to regulate appetite in real time and over the longer term.
How the Gut-Brain Axis Controls Appetite
At the center of this process is the gut-brain axis, a bidirectional communication pathway that links the digestive tract to the brain through hormonal signaling, nerve pathways, and metabolic feedback. The hypothalamus, located deep within the brain, integrates these incoming signals and determines whether to stimulate or suppress appetite.
Two key neuronal groups sit at the core of this regulation:
- NPY/AgRP neurons activate hunger, pushing you to seek food.
- POMC/CART neurons promote satiety and reduce intake.
These neurons constantly receive input from the gut and other organs, adjusting appetite minute by minute. It is a complex, dynamic system rather than a simple on-off switch.
Hunger Hormones That Influence When You Eat
Your gut acts like an endocrine organ, releasing a series of hormones in response to fasting and feeding. These hunger and satiety hormones travel through the bloodstream and communicate directly with the brain. Here are a few key players:
- Ghrelin: Produced in the stomach, ghrelin is often called the hunger hormone. Its level rises before meals and falls after eating. Ghrelin not only makes you hungry but also activates reward pathways that make food more appealing.
- Cholecystokinin (CCK): Released by cells in the upper small intestine when fat and protein enter, CCK provides one of the earliest “I have eaten” signals. It slows gastric emptying and stimulates vagal nerve signals that promote satiety.
- GLP-1 (Glucagon-like peptide 1) and PYY (Peptide YY): These hormones are released further down the digestive tract, mainly from the ileum and colon, as nutrients progress through. They sustain fullness, slow gastric emptying, and suppress appetite for several hours after eating. GLP-1 has received enormous attention recently as the target of medications such as semaglutide and tirzepatide.
- GIP (Gastric inhibitory polypeptide): Another incretin hormone that plays a supporting role by enhancing insulin secretion and modulating appetite. Newer combination therapies target both GLP-1 and GIP for greater effect.
- Bile acids: Beyond aiding digestion, bile acids activate receptors in the gut such as TGR5 and FXR that can influence GLP-1 secretion and energy metabolism, adding another layer to appetite control.
The timing and balance of these hormonal signals help determine how hungry you feel before a meal and how satisfied you feel afterward.
The Role of the Vagus Nerve in Appetite and Feeling Full
The vagus nerve is the primary fast communication pathway between the gut and the brain. It transmits real-time information about the mechanical stretch of the stomach and bowel, as well as details about the chemical environment, helping the brain initiate the process of satiation. When food enters the stomach, stretch receptors activate and send real time neural signals that contribute to the decision to stop eating.
Specialized sensory cells in the gut lining also respond to nutrients, releasing neurotransmitters and hormones that add additional layers of signaling. These hormonal effects reach the brain more slowly through the bloodstream and play a greater role in satiety, the longer-lasting feeling of fullness that develops after a meal. Eating slowly gives the rapid vagal signals and the slower hormonal pathways time to work together, improving the body’s ability to sense and respond to food intake.
How the Gut Microbiome Affects Hunger and Satiety
The trillions of bacteria living in your gut play a critical role in appetite regulation and digestion. They produce short-chain fatty acids such as acetate, propionate, and butyrate when they ferment dietary fiber. These short-chain fatty acids stimulate the release of PYY and GLP-1, reinforce gut barrier integrity, and may even communicate directly with the vagus nerve.
Certain bacterial profiles are associated with increased satiety hormone production, while others may promote overeating. Although this field is still evolving, it is increasingly clear that the microbiome is not just a passive passenger. It is an active metabolic organ influencing how hungry or full you feel.
How Sleep, Stress, and Circadian Rhythms Influence Appetite and Fullness
Woman working late at home
getty
Appetite signaling does not operate in isolation. Everyday factors such as sleep, stress, and light exposure can quickly disrupt or amplify the same hormonal pathways that regulate hunger and fullness. Research over the past two decades has shown that these factors can shift levels of leptin, ghrelin, and cortisol, and alter how sensitive the brain remains to these signals.
Sleep deprivation
Even a few nights of inadequate sleep can alter appetite hormones in measurable ways. Landmark research from the University of Chicago published in Annals of Internal Medicine in 2004 found that restricting sleep to four hours per night for just two days reduced circulating leptin, the hormone that signals fullness and helps regulate body weight, and raised ghrelin, which stimulates hunger. A large population study published in PLOS Medicine the same year confirmed these findings, linking short sleep duration with higher ghrelin, lower leptin, and ultimately a higher body mass index. Later research published in The Journal of Clinical Endocrinology & Metabolism in 2012 showed that sleep loss also heightens brain reward responses to high-calorie foods, suggesting that the brain becomes more reactive to food cues when tired. This combination of lower leptin signaling, higher ghrelin, and greater reward sensitivity creates ideal conditions for overeating.
Although leptin primarily regulates longer-term energy balance and body weight, these studies show that short-term changes in leptin can influence appetite and fullness during periods of sleep loss or stress, linking it to both acute and chronic regulation of intake.
Stress and cortisol
Under both acute and chronic stress, the adrenal glands release cortisol, a hormone that mobilizes energy but also influences appetite and food choice. Research from the University of California, San Francisco, published in Psychoneuroendocrinology in 2001, found that elevated cortisol increases appetite and preference for energy-dense comfort foods, particularly those high in sugar and fat. Chronically high cortisol levels can also impair leptin signaling, making it harder for the brain to recognize satiety.
Circadian rhythm misalignment
Timing matters as much as quantity. Research from Harvard Medical School published in Proceedings of the National Academy of Sciences in 2009 demonstrated that circadian misalignment, such as during shift work or frequent time zone changes, disrupts normal cycles of leptin and ghrelin. Leptin levels drop and ghrelin rises at times when the body should be resting, producing hunger at night and diminished satiety after meals. These hormonal changes occur even when total sleep duration is adequate, underscoring how sensitive appetite regulation is to light exposure and meal timing.
Together, these studies reveal that sleep, stress, and circadian rhythm act as powerful short-term modulators of appetite. Each can lower leptin or blunt leptin sensing, raise ghrelin, and alter cortisol balance, leading to increased hunger and stronger cravings. In everyday terms, being tired, stressed, or off schedule does not just make eating more tempting. It changes the underlying biology that governs when and how much you want to eat.
Hedonic Hunger vs Homeostatic Hunger
Dessert temptation after dinner
getty
Not all hunger comes from biological need. Homeostatic hunger arises from true energy requirements and gut-brain signaling, although this can become dysregulated as we will discuss in subsequent installments. Hedonic hunger, in contrast, is driven by the brain’s reward circuits, often triggered by hyper-palatable foods that combine sugar, fat, and salt in ways that override natural satiety mechanisms.
Hedonic hunger is largely mediated by dopamine, the neurotransmitter that reinforces behaviors linked to pleasure and reward. When you eat highly palatable foods, dopamine is released in brain regions such as the nucleus accumbens, creating a sense of satisfaction and teaching the brain to repeat the behavior. Over time, cues such as sight or smell can trigger dopamine release even before eating begins, intensifying cravings. Research from the National Institute on Drug Abuse published in Nature Neuroscience in 2011 demonstrated that these dopamine responses can occur even in people who are not physiologically hungry, helping explain why food cravings often persist despite fullness.
This distinction matters. You might feel hungry for dessert after a large dinner not because your body needs calories, but because your brain’s reward system is still activated. Modern food environments exploit this biological gap relentlessly, keeping appetite and cravings constantly activated.
Hunger Hormones vs Long-Term Weight Regulation
These short-term appetite mechanisms explain why you get hungry, why fullness takes time to register, and why sleep and stress can throw your eating off track. But they do not tell the whole story of why people gain or lose weight over the long term.
Your body also has a long-term thermostat that regulates weight through hormones such as leptin and insulin, adjusting both appetite and energy expenditure to maintain a body weight set point. That system, how it works, and why it often drifts upward, is the focus of the next article in this series.
The Takeaway
Hunger and fullness are not voluntary experiences. They reflect coordinated communication between the gut, brain, and hormones that operate largely outside conscious control. Recognizing how these pathways work helps explain why hunger can feel unpredictable and why approaches that respect the body’s internal cues are more effective than those that fight them.